Cesarean scar ectopic pregnancy- MRI
History – 28 yrs age gravid female with
history of past LSCS delivery. USG done about 1 month back suggesting relative
low intrauterine pregnancy (images not available). Patient did not want to continue the
pregnancy due to unknown reasons & hence MTP was attempted following which
minimal PV bleed occurred without any definite expulsion of products.
Patient was referred for MRI pelvis to assess the present status of the gestation
sac & to look for the status of uterine scar from previous LSCS.
-
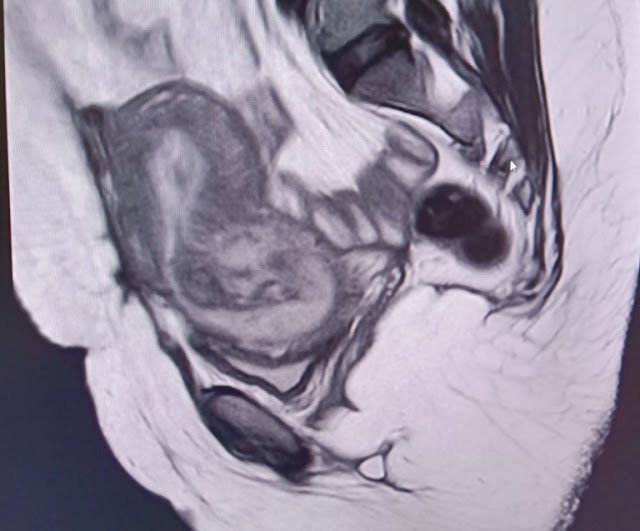
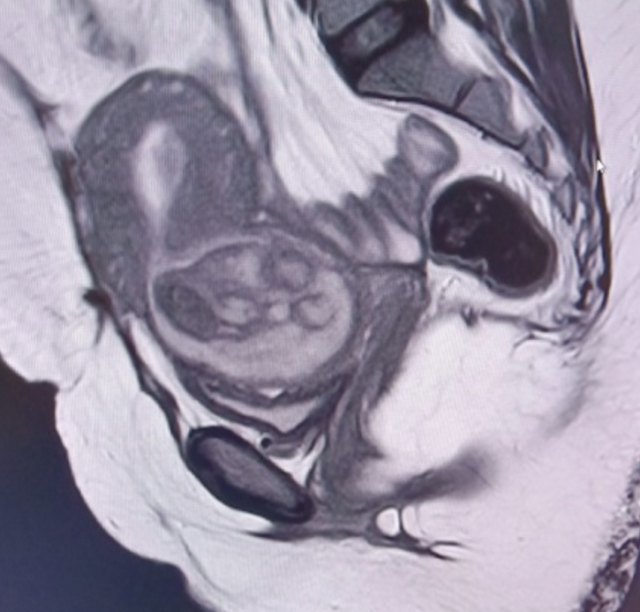
T2 images ( sag , cor &
axial) – show mixed signal fairly well defined oval shaped lesion in the low
anterior uterine segment extending into the cervix causing dilatation of the
cervix along with inferior bulge of the lower cervical lips causing effacement
of the posterior fornix of vagina with possible endocervical canal extension. Superiorly
thin extension of the T2 hypointense signal from the lesion into the
endometrial cavity was also seen. Lesion appears iso to hyperintense in T1 with
marked blooming areas within the lesion in GRE extending into the endometrial
cavity suggesting hemorrhagic contents in the lesion.
-
Focal grossly thinned out
anterior myometrium seen in the low uterine seg
-
ment ( LUS) showing broad
contact with the above mentioned lesion in LUS & cervix. No defect or any rupture was seen in the
uterine scar. No collection or any free fluid was seen in the parametrium.
-
Thick adhesion bands with T2 hypointense signal were seen between the anterior wall of
uterus & adjacent abdominal wall .
These MR imaging findings suggest lesion with
hemorrhagic contents in LUS with extension into the cervix causing its
dilatation along with hemorrhage within
the endometrial cavity – likely
retained products of conception ( in view of previous USG findings)
& broad contact of lesion with anterior LUS scar suspicious for cesarean
scar ectopic pregnancy.
— Intra op findings - Crumpled sac like structure with hemorrhages & with dense
adherence to the thinned out uterine scar which was cleared & myometrium
was resutured.Uterus was preserved in the surgery & diagnosis of Cesarean scar ectopic pregnancy along with
RPOC was made.
— Cesarean scar ectopic pregnancy
(CSEP) or Cesarean
scar pregnancy (CSP) is a rare form of ectopic pregnancy resulting from
implantation of a blastocyst within myometrial scar tissue (old uterine scars)
in the anterior lower uterine segment (LUS) at the site of prior Cesarean
section.
— It is considered amongst the rarest type of ectopic pregnancy,
although some do not include it in the category of ectopic pregnancy as
implantation occurs within the uterus itself.
— Incidence is on rise due to increasing numbers of elective Cesarean
sections as well as improved detection with transvaginal ultrasound
(TVUS).
— Estimated incidence is about 1 per 1,800-2,226 pregnancies,
exceeding than that of cervical ectopic pregnancies.
Clinical presentation -
— Vaginal bleeding and abdominal pain.
— Severe acute abdominal pain
or heavy vaginal bleeding are concerning for impending rupture.
— Hemodynamic instability may indicate rupture of CSP through the
myometrium.
— Up to 40 percent of patients may remain asymptomatic.
— CSP can present at any time during gestation.
PATHOLOGY-
— Myometrial defects result from prior Cesarean section or after other
uterine interventions like, dilatation and curettage ( D & C), myomectomy,
hysteroscopy, and metroplasty.
— Poor vascularity in the LUS impairs healing of scar and contributes to the formation
of small myometrial defects in which the trophoblast may implant.
— Poor healing can result in a focal thinning of the scar, which may be more
susceptible to implantation of the gestational sac at this point rather than in
the endometrial cavity.
— Women who undergo multiple Cesarean sections are at increased risk
of scar implantation due to increased scar surface area.
DIAGNOSIS
-
TVUS - modality of choice for diagnosis of CSP in
the first trimester. A sagittal view along the long axis of the uterus
through the plane of the gestational sac allows accurate localization within
the anterior LUS.
The following
sonographic criteria have been proposed for diagnosis of CSP:
— empty uterine cavity with clearly visualized endometrium;
— empty cervical canal;
— gestational sac in the anterior Low uterine segment and
— absent or deficient intervening myometrium between the gestational
sac and bladder wall, typically <5mm .="" o:p="">
— High velocity (>20cm/sec), low-impedence peritrophoblastic color
Doppler flow (pulsatility index <1 0.5="" 3.1="" also="" and="" been="" cases="" described="" flow="" have="" implantation.="" in="" index="" o:p="" of="" peak="" ratio="" resistive="" scar="" systolic:diastolic="">
Noncontrast MRI
— Better demonstrate involvement of adjacent organs such as the
urinary bladder and in orienting the surgeon.
— In more advanced pregnancies, MR optimally demonstrates findings of
placenta accreta spectrum, which may include thinning or absence of the
subplacental myometrium, aberrant vessels, focal bulging of the uterine
contour, and invasion of the urinary bladder or anterior abdominal
wall. The presence of T2 hypointense, irregular intraplacental bands
analogous to the vascularized lacuna seen on ultrasound, is strongly associated
with abnormalities of placentation.
DDs-
— Cervical ectopic pregnancies - located within cervical
stroma, adjacent to the cervical canal.
— Normal low intrauterine pregnancies - seen above the internal os and should have normal-thickness of overlying myometrium.
— Spontaneous abortion - gestational sac will often appear
collapsed or irregular, lack normal surrounding color Doppler flow.
Management -
— Management decisions depend on gestational age and size, severity of
implantation anomaly, clinical stability, and patient desire for future fertility.
— Ultrasound-guided methotrexate
injection has emerged as the treatment of choice.
— Isolated dilatation and curettage is generally contraindicated due high risk of
incomplete evacuation, uterine rupture and injury to the bladder.
— Termination of pregnancy in the first trimester is generally
recommended due to the high rate of complications which later require hysterectomy .
— Patients who do not respond to conservative measures may require
laparoscopic or open excision, which allows for concurrent revision of the
Cesarean scar to minimize risk of recurrence.
Cesarean scar ectopic pregnancy- MRI
 Reviewed by Sumer Sethi
on
Friday, March 20, 2020
Rating:
Reviewed by Sumer Sethi
on
Friday, March 20, 2020
Rating:
 Reviewed by Sumer Sethi
on
Friday, March 20, 2020
Rating:
Reviewed by Sumer Sethi
on
Friday, March 20, 2020
Rating:














No comments:
Post a Comment